
How Well Does Your Practice Adhere to Anesthesia Guidelines?
March 27, 2025
How to Add Dental Sedation Services Without Disrupting Workflow?
October 8, 2025In May 2023, South Carolina partially repealed its Certificate of Need (CON) requirements for Ambulatory Surgery Centers (ASCs), eliminating key barriers to opening and expanding these facilities. As expected, the state has since seen a notable uptick in ASC construction and activity.
But this rapid growth is now facing a critical challenge: a worsening anesthesiologist shortage. As one CRNA from Arizona put it, “It seems like every street corner has a new surgery center going up, and the number of procedures requiring anesthesia is growing faster than we can train new providers.”
This is the reality ASCs and outpatient surgery centers are facing today. Demand is rising, facilities are opening, but the workforce needed to deliver safe, consistent ambulatory anesthesia is under strain. The good news? With the right approach, ASCs can mitigate that challenge.
The Demand for Anesthesia Providers Is Growing
The need for qualified anesthesia providers has never been more pressing, driven by several factors that are reshaping the healthcare landscape:
- Aging Population:
The aging population is intensifying the need for anesthesia providers, as older adults often require more procedures involving monitored sedation or general anesthesia. - Increasing Complexity of Surgeries:
Modern surgeries are in higher demand and are also more intricate and technologically advanced. However, with the added complexity comes greater risk, making qualified anesthesiologists even more important for anesthesia safety and recovery outcomes. - Rise of ASCs and Outpatient Centers:
Outpatient surgery centers are growing in popularity, offering patients a more convenient and cost-effective alternative to traditional hospitals. But as demand increases, so does the need for qualified anesthesia providers, further straining an already limited talent pool.
Anesthesiologist Employment Outlook
How Many Anesthesiologists Are There in the U.S.?
According to Statista, as of January 2025, there were 53,548 active anesthesiologists in the U.S. However, workforce projections indicate a growing supply-demand gap that should concern every hospital, outpatient center, and ASC manager. The Association of American Medical Colleges (AAMC) projects a shortage of 12,500 anesthesiologists — nearly 30% of current staffing levels — by 2033.
Why Is There a Shortage of Anesthesia Providers?
Several systemic issues are contributing to this alarming trend:
Aging Workforce:
Not only the population in general is aging, but so are the anesthesiologists. In 2020, the average age of anesthesiologists was 52.6, indicating that many are expected to retire within the next decade.
Lengthy Recruitment Cycles:
Surgical procedures are the core service offering for ASCs and many outpatient centers, yet filling a permanent anesthesiologist position takes an average of 120 days. This extended timeline creates operational disruptions and financial strain that many ASCs struggle to manage effectively.
Burnout and Attrition:
Roughly 50% of anesthesiologists report burnout, and 61% said they’d even accept lower pay for a better work-life balance. These statistics highlight a growing dissatisfaction that fuels turnover and reinforce the urgent need for healthcare facilities to create more sustainable practice environments.
Training Bottlenecks:
Even as demand grows, the pipeline for training new anesthesiologists remains severely constrained. Nearly 44% of medical school graduates who applied for anesthesiology residencies last year failed to match, highlighting a critical bottleneck in developing the next generation of anesthesiologists.
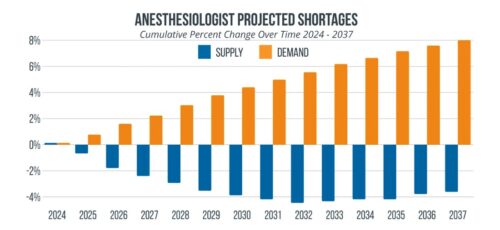
Source: Medicus Healthcare Solutions
What Does the Anesthesiologist Shortage Mean for ASCs and Outpatient Centers?
The anesthesiologist shortage is a growing national concern, but it is particularly disruptive for ASCs and outpatient centers. These implications include:
Financial Pressures:
Amid an 8.2% decline in anesthesia reimbursement over the past decade, the cost of hiring anesthesiologists has continued to rise. The competition for a shrinking pool of providers, along with growing demands for better compensation and work conditions, has driven anesthesiologists’ salaries up by as much as 40%.
Operational Delays:
The limited availability of anesthesiologists leads to delayed or canceled procedures, longer wait times, and reduced capacity for complex surgeries, which also translates into financial strain.
Quality Concerns:
With insufficient anesthesiologists to hire, many facilities are turning to locum tenens or less-experienced providers to fill staffing gaps. However, this approach risks quality care, deviates from standard anesthesia guidelines, and increases the likelihood of complications. All of the above can ultimately harm a facility’s reputation and raise liability concerns.
Staff Burnout:
Existing anesthesiologists within these facilities may face increased workloads and pressure, potentially leading to burnout and turnover. This creates a vicious cycle where workforce shortages lead to increased stress, which in turn drives more providers away from the profession.
CRNAs: A Vital Part of the Solution
While the anesthesiologist shortage presents significant challenges, CRNAs offer a compelling solution.
How Many CRNAs Are in the U.S.?
According to the National Board of Certification and Recertification for Nurse Anesthetists, there are currently over 62,000 CRNAs in the U.S., and interestingly enough, their employment trajectory is the opposite of anesthesiologists’. The U.S. Bureau of Labor Statistics projects a 38% job growth for CRNAs by 2032, far outpacing most other roles in healthcare.
CRNAs Can Meet the Demand
Several trends make CRNAs an ideal solution to the anesthesiologist shortage:
- Strong and Growing Workforce: With over 62,000 practicing CRNAs (already outnumbering the 53,548 anesthesiologists), the CRNA workforce is not only larger but also expanding.
- Younger and More Stable: According to the American Association of Nurse Anesthesiologists, the average CRNA is 47.5 years old, and only 12% plan to retire by 2027.
- Growing Autonomy: In 27 states, including North Carolina, CRNAs are permitted to practice independently or with reduced physician oversight. This allows facilities to maintain high-quality anesthesia care without relying on multiple anesthesiologists.
NovaSed: Your Partner in Anesthesia Excellence
Anesthesia staffing doesn’t have to be a constant challenge. As the industry evolves, more and more facilities are turning to CRNAs, and NovaSed is proud to lead that movement.
NovaSed was founded by CRNAs and employs over 20 highly trained CRNAs serving facilities throughout the Carolinas. We provide reliable, high-quality, full-spectrum anesthesia services, so you don’t have to worry about recruitment delays, operational slowdowns, burnout, or the rising costs tied to traditional staffing models.By partnering with NovaSed, your facility can maintain uninterrupted operations, take on more cases, and ensure the highest standards of patient safety. Let’s talk about how we can partner with you to deliver the care and peace of mind you and your patients deserve.


