Ensuring Anesthesia Safety: A Quick Guide for Medical Clinics
December 6, 2024
How to Choose the Right Anesthesia Provider for Your Practice?
January 13, 2025Modern dentistry requires more than clinical expertise; it demands a focus on patient comfort and trust. For many, visiting the dentist is an intimidating experience, filled with anxiety and uncertainty (somewhat like when seeing a therapist). On top of that, patients today expect more than just treatment; they want care that addresses their fears and makes the process as stress-free as possible.
One powerful way dentists can bridge this gap is through sedation dentistry. By offering tailored sedation for dental work, dentists can transform a potentially terrifying experience into one that puts both patients and practitioners at ease.
Types of Dental Sedation
Before we explore some practical considerations when developing a dental sedation program for patients or general sedation guidelines for dental practices, let’s quickly review the common types of dental sedation.
Local Anesthesia
While not considered dental sedation, local anesthesia is among the most common types of pain management care in dentistry. Unlike the other types of sedation for dental work discussed below, which induce relaxation or sleepiness, local anesthesia numbs the area where the anesthetic (usually Lidocaine) is injected. Local anesthesia can be delivered by dentists, hygienists, periodontists, or other qualified team members.
Nitrous Oxide (Laughing Gas)
Nitrous oxide is the mildest dental sedation model and one of the most widely offered methods, with approximately 60% of dentists incorporating it into their practice. Administered through a nasal mask or nosepiece, it induces a calm, relaxed state within minutes, but its effects also wear off quickly once the gas supply is stopped.
Oral Sedation
This form of minimal sedation is popular among patients as it eliminates the need for needles or injections. Unlike nitrous oxide, its effects last longer, making it suitable for more extended procedures. For the sedation to kick in, patients take a sedative pill (most often triazolam or another drug from the benzodiazepine class) either the night before or about an hour before their appointment. Dentists must carefully evaluate the patient’s medical history to determine the most appropriate sedative.
Intravenous (IV) sedation
IV sedation provides the deepest level of conscious sedation available in dental practices. Sedatives are administered directly into the bloodstream, and continuous monitoring of the patient’s vital signs is necessary during and after the procedure to ensure patient safety. While IV sedation can ease treatment for anxious patients, it also presents logistical challenges for dentists who must balance sedation monitoring with procedural demands. Also, dentists must have advanced training and certification due to this sedation model's complexity.
General Anesthesia
Reserved for complex dental/oral procedures or patients with extreme needs, general anesthesia involves inducing complete unconsciousness, rendering the patient unable to feel or respond during the procedure. Dentists rarely perform this type of sedation in-office due to its specialized nature and the stringent safety protocols. Instead, general anesthesia is typically limited to hospital or ambulatory surgery center (ASC) settings and is usually administered by an anesthesiologist or anesthesia-trained professional.
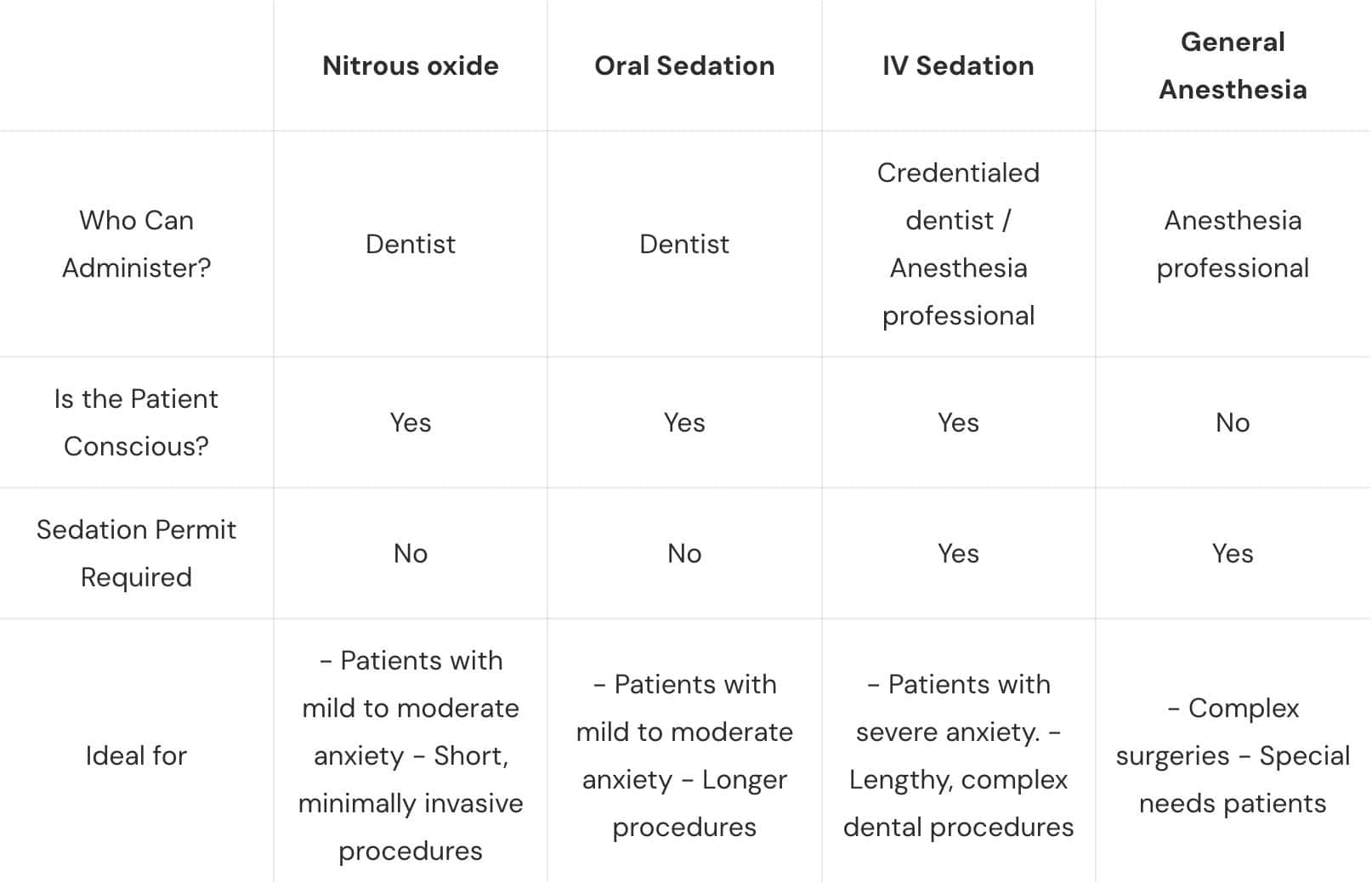
Here’s a summary of the common types of dental sedation:
Versatility in Sedation Options Can Grow Your Practice
Over the past decade, we’ve seen a 20% increase in the adoption of sedation techniques in dental offices, potentially as a solution for the third of Americans suffering from dental anxiety. However, dental teams that can skillfully implement multiple sedation techniques into their practice not only provide better patient care but also gain some strategic advantages:
- Broader patient base through the ability to address a wider range of patient needs.
- Increased revenue through the ability to perform more complex procedures that require deeper sedation levels.
- Enhanced patient retention through improved comfort and trust building between the clinical team and the patients.
Factors to Consider When Developing A Sedation Strategy
Dental practices with versatile sedation offerings will need to develop a tailored dental sedation strategy for each patient. To do it effectively and safely, dentists must carefully evaluate the following three factors:
1. Evaluating Patient Candidacy for Sedation
When selecting the appropriate sedation method, dentists must thoroughly assess each patient’s unique needs and health profile. This evaluation should include a detailed review of the patient’s medical history, current medications, allergies, age, weight, anxiety levels, and personal preferences.
Certain health conditions and medical histories may introduce risks that influence the choice of sedation. For example, patients taking medications for heart or respiratory conditions may need to avoid specific sedatives. Similarly, patients with a history of adverse reactions to sedative medications or pregnant patients may require alternative approaches to pain management.
2. Evaluating Procedural Demands
The nature of the dental procedure is another critical factor to consider when developing a sedation plan. Longer, more invasive, or more complex procedures often require deeper levels of sedation to ensure patient comfort and cooperation throughout. Conversely, for shorter and minimally invasive treatments, minimal sedation might suffice. Specifically, it’s recommended to consider:
- Procedure’s Duration: Extended treatments may benefit from IV sedation to maintain patient relaxation for a prolonged period.
- Procedure’s Complexity: Surgical interventions, such as wisdom tooth extractions or dental implants, often require deeper sedation methods to ensure the patient remains still and calm.
3. Evaluating Your Practice Readiness for Dental Sedation Administration
Beyond patient evaluation, the practice’s capacity to administer sedation effectively and safely plays a critical role. Here’s what you should consider:
- Anesthesia Staffing: Does your team have the expertise and resources to support IV sedation? If not, consider minimal sedation options or collaborate with an anesthesia professional for higher levels of sedation.
- Sedation Permitting: In the Carolinas, dentists must have a valid sedation permit to administer IV sedation, even if they are not the ones administering it. Does your practice comply with state regulations? If not, you might want to get one.
- Staff Training: Before offering IV sedation at your clinic, it’s recommended to ensure all team members are certified in Basic Life Support (BLS), Advanced Cardiac Life Support (ACLS), or Pediatric Advanced Life Support (PALS).
- Guidelines for Risk Management: Before administering any type of sedation, especially IV sedation, ensure your practice has well-established internal policies for sedation administration, patient monitoring, and emergency preparedness.
Which Sedation Dentistry Approach is Right for Your Practice?
When it comes to sedation administration, there’s not a one-size-fits-all solution. Dental practices should aim to offer a variety of sedation options to meet their patients’ diverse needs. That said, while diversifying sedation options can significantly enhance patient care, the golden rule remains: only administer sedation techniques your team can confidently and safely implement.
To ensure your practice has the highest level of sedation support, NovaSed is here to help. Our experienced CRNAs provide comprehensive dental sedation services tailored to dental clinics, including dedicated sedation teams, customized sedation guidelines, and assistance with sedation permitting. Contact us today to enhance your practice’s sedation capabilities while maintaining the highest standards of patient safety.